In the middle of the face stands the nose. However, it is rarely the first feature one notices, unless it stands out due to size or shape.
When looking at someone, emotions are primarily conveyed through the mouth-eye triangle. Unfortunately, a nose that is too wide, too strong, deviated, too flat, too round, or bifurcated can draw attention. The nose may even hinder the transmission of emotions; for instance, a sharply pointed nose can harden the face and disrupt its harmony. Understanding that a disharmonious nose often has suboptimal respiratory function is crucial.
Rhinoplasty aims to integrate the nose into the face by shaping each structure according to the patient's desires, genetic factors, facial anatomy, and the surgeon's technical realities.
The nose should be as harmonious as possible with facial proportions and aesthetically pleasing, never forgetting its primary function of ensuring breathing. The nose must be entirely natural, as an unnatural appearance may once again capture attention and distort the emotions perceived by observers.
Therefore, as many rhinoplasties exist as there are different faces.
Our collaborative work begins by identifying problematic areas on your nose. It is rare for the entire nose to be displeasing, and anatomically, there are often "very beautiful" areas on "unattractive" noses.
To create a photo project using morphing software, we need to:


After the first consultation, my charming assistants will provide you with a summary, including the rhinoplasty document from SOFCPRE, the septoplasty document from SFORL, your photo project if desired, and a detailed quote including surgical, anesthesia, clinic fees, and postoperative consultations.
Partial health insurance coverage limited to the treatment of nasal obstruction may be requested if significant respiratory problems have been diagnosed.
Thus, a minimum of two consultations is necessary to establish both a human and medical connection. The postoperative period and risks will be highlighted in the first consultation. Edema is systematic and moderate in the first few days, with bruises being rare. The specific risk of rhinoplasty is a healing defect that may lead to a minor surgical revision in less than 5% of cases, often limited to local anesthesia.
A final consultation will be conducted the day before, two days before, or the morning of the surgery to perform LED to prepare the tissues for surgery and minimize edema and bruising if any.
The surgery takes place at the Saint-George Clinic in Hall 2, in a dedicated aesthetic service located on the bridge above the parking lot. Both the surgical and service teams are specifically trained in pre and postoperative aesthetic care.
The duration of general anesthesia is usually between 1.5 and 2 hours.
Rhinoplasty is typically performed on an outpatient basis, meaning you enter and leave the clinic on the same day. For this, someone must bring you and take you back. You are not allowed to drive for 24 hours after general anesthesia. It is also mandatory to have an adult with you on the first night.
Postoperatively, pain is minimal to nonexistent, with only paracetamol (Tylenol) needed for a few days. Antibiotics will be necessary for seven days.
At the clinic, cold compresses are placed on the eyes to minimize swelling around the eyes. You will replace them with frozen peas for 20 minutes five times a day and at bedtime for the first few days. Bruises under the eyes are rare and disappear quickly. A social eviction of 7 days is recommended.
Upon waking, there is a small greasy cotton in the nostrils (definitely not a tampon!), which you will easily remove the next morning.
A small thermoformed splint is placed on the nose for 7 days. If a respiratory procedure is performed simultaneously, thin silicone sheets are placed on either side of the nasal septum. They do not obstruct breathing, and their removal is painless. Their removal takes place on the 7th day, simultaneously with the splint removal; it is painless.


The swelling of the nose will decrease gradually on the nose and inside the nose, sometimes with a feeling of a partially blocked nose initially. Thus, upon splint removal, you often already appreciate your nose in profile and three-quarters, but not yet from the front. The slow reduction of swelling, especially in the frontal view, will help ensure that those around you do not realize that surgery has been performed.
There is approximately 30% swelling at one month, 20% at 3 months, 10% at 6 months, 5% at one year, and the result is definitive at two years. The swelling will take the longest to resolve in the lower part (tip and junction of the tip and dorsum of the nose), especially if the skin is thick and it is a secondary rhinoplasty.
The nose is completely consolidated between 8 and 12 weeks, so no contact sports should be played during this time or heavy glasses should be worn. Light glasses are allowed after one week. Medical follow-up is essential to monitor and guide this slow healing process. After splint removal, specific patient-specific massages will be taught, performed on average three times for five minutes each day during 3 months.
Before the surgery, the schedule for postoperative appointments will be provided to you. The calendar includes a minimum of seven checks on D7, M1, M2, M3, M6, Y1, and Y2. The goal of this follow-up is to minimize the risk of surgical revision (<5%), guide massages, and, if necessary, perform small injections of corticosteroids to expedite edema reduction or hyaluronic acid to prevent adhesions.
Scars may be located differently depending on the type of rhinoplasty.
Mini-invasive rhinoplasty is part of the preservation rhinoplasty family, aiming to minimize tissue aggression during surgery and preserve the unique characteristics of each nose to harmonize it with the face. I have been developing this technique since 2011, and now, mini-invasive rhinoplasty represents over 90% of my rhinoplasties.
Technically, there is no scar on the skin; dissection occurs closest to the cartilage and bone, preserving all subcutaneous tissues to avoid irregularities. Small ligaments are also preserved, allowing for better skin redraping aesthetically and avoiding respiratory discomfort functionally.
At the nasal tip, shaping is done through suturing and repositioning techniques with minimal cartilage resection, providing both aesthetic and functional benefits.
Structural rhinoplasty is suitable for noses requiring major reconstruction of the tip, usually secondary rhinoplasties or tips with significant asymmetries.
Technically, a scar is made at the base of the columella (pillar separating the two nostrils). Cartilage grafts are taken from the septum inside the nose or behind the ears to strengthen or recreate the tip's architecture.
Postoperative recovery is generally longer, especially in terms of edema.
Medical rhinoplasty is a camouflage rhinoplasty, involving enhancing specific areas of the nose to minimize a bump, lift a tip, or correct an irregularity. Before any medical rhinoplasty, besides checking for any medical contraindication to hyaluronic acid injection, it is crucial to be sure about wanting and/or being able to increase the overall size of the nose.
A good indication, for example, is a small nose with a bump or a drooping tip, making it a suitable case for medical rhinoplasty.




























Correction of Nasal Obstruction and Drooping Nose
The patient had right nasal obstruction due to a deviated septum, along with a bump and a drooping nasal tip. Her vertically asymmetric drooping tip was associated with a right external valve, causing occlusion of the right nostril during forced inspiration. A conservative anatomical rhinoplasty was performed to lift the tip, straighten the septum, address both internal and external valve issues, and remove the bump.
This technique addressed both morphological and functional issues simultaneously, with no scars and a simple, quick recovery. Result after one year: a happy patient.



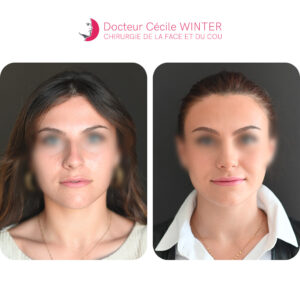
Correction of Nasal Obstruction and Aesthetic Improvement
The patient was troubled by a permanent right nasal obstruction causing migraines, as well as a deviation, a bump, and an asymmetric base morphologically. A conservative anatomical rhinoplasty was performed a year ago, with a smooth postoperative course. Nasal edema will gradually subside, allowing the nose to refine slowly over time, depending on the skin type, between one and two and a half years. This gradual change prevents acquaintances from noticing the rhinoplasty. Additionally, this technique preserves balance points such as the height of the nasal root, which is crucial for the intensity of the gaze. The patient is breathing well and looks superb.



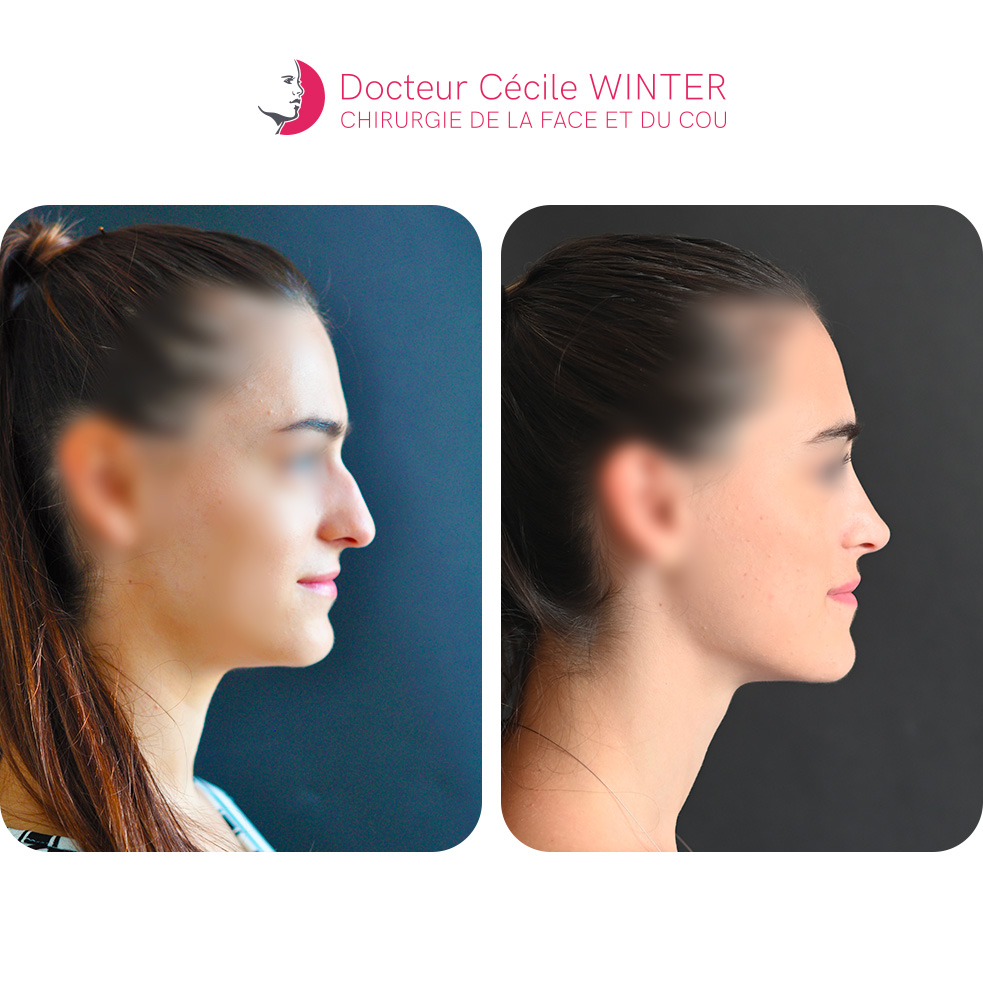
Correction of Prominent Nose and Functional Improvement
Thank you to our wonderful patient for agreeing to share the photos. The patient was troubled by a prominent nose with a long, drooping tip and experienced breathing difficulties during exertion, associated with an internal septal deviation. A scarless conservative anatomical rhinoplasty was performed, addressing the bump, hyperprojection, and length of the septum, and rotating the tip upward to provide support, especially when smiling. The patient is happy with the results both functionally and aesthetically.



Correction of Drooping Nose and Breathing Improvement
The patient had a very large, drooping nose under tension, with breathing difficulties during exertion due to internal and external valve syndrome. A scarless conservative anatomical rhinoplasty was performed, with a smooth postoperative course. The goal was to reduce the height, septal length, and bump to relieve nasal tension and improve breathing. The tip was lifted and stabilized simultaneously. Today, the patient looks wonderful and feels great.



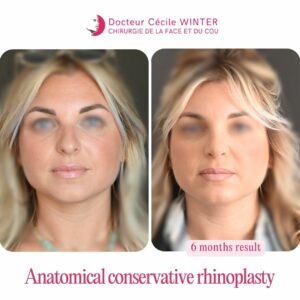
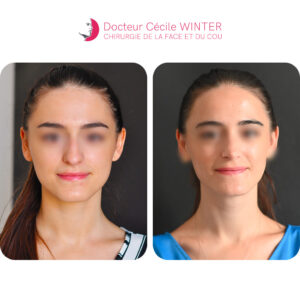
Conservative Anatomical Rhinoseptoplasty for Nasal Obstruction and Septal Deviation
Patient with intermittent obstruction due to bilateral internal and external valve syndromes, predominantly on the right side. Nasofibroscopy revealed a deviated septum and inferior turbinate hypertrophy. Morphologically, her septum was high and long with a normally positioned root and a tip deviated to the right and vertical.
A conservative anatomical rhinoseptoplasty was performed 6 months ago, with no visible scars. The deviation and valve syndromes were corrected. This led to morphological improvement with the disappearance of the hump, a better-supported and elevated tip, and a centered, well-defined lobule. The patient is radiant and breathes well.



Functional and Aesthetic Correction of the Nose
The patient experienced discomfort due to a prominent nose with a hump, a poorly defined drooping bulbous tip, an asymmetrical and pinched middle third, and a deviated septum causing functional breathing difficulties similar to an internal valve syndrome. Additionally, there was tip asymmetry with bilateral external valve syndrome, more pronounced on the left. A scarless conservative anatomical rhinoplasty was performed to correct the septum hypertrophy, the middle third, the hump, and to refine and strengthen the architecture of the tip, improving breathing and eliminating discomfort during forced inspiration. One year post-operation, the patient is breathing well and is delighted with the result!



Correction of Nasal Obstruction and Nevus
This patient was bothered by permanent nasal obstruction due to allergies and a deviated nasal septum, as well as a nevus at the inner corner of the left eye that had recently increased in size. A conservative anatomical rhinoplasty was performed without visible scars to correct her deviated, overly projected nose, her vertical tip, and hypertrophy of the inferior turbinates. The postoperative course was straightforward, and no scars were noted except at the nevus site. The patient is pleased both functionally and aesthetically.



Correction of Long, Convex Nose with Respiratory Improvement
The patient was troubled by a long, convex, and poorly defined nose, along with breathing difficulties due to hypertrophy of the inferior turbinates. A conservative anatomical rhinoplasty was performed 4 years ago, correcting both functional and morphological issues at the tip, nasal cavities, and dorsum, without any scarring. A small bony fragment on the dorsum appeared at 6 months, requiring a minor touch-up under local anesthesia at one year. Today, the patient is delighted with the functional and aesthetic results. It is always a joy to see our patients many years later



Conservative Anatomical Rhinoplasty for an Over-Projected Nose
Patient troubled by an over-projected nose under tension, with secondary breathing difficulties. In addition to a deviated nasal septum, she had a pinched middle third and a bulbous tip, causing functional issues. A conservative anatomical rhinoplasty was performed a year ago, without visible scars, with a smooth recovery. Today, the patient breathes well and is satisfied with the result.



Conservative Anatomical Rhinoplasty for Post-Traumatic Nasal Asymmetry
Patient with post-traumatic nasal asymmetry, inferior turbinate hypertrophy, and internal valve syndrome causing significant breathing problems. In addition to severe deviation of the nasal septum, there was a dorsal hump and a long, asymmetrical tip, leading to functional issues.
A conservative anatomical rhinoplasty was performed 7 days ago, with no visible scars, simple recovery, no packing, and no pain or bruising due to the minimal approach and minimal dissections of the conservative anatomical rhinoplasty



Rhinoseptoplasty for Bilateral Nasal Obstruction and Wide Drooping Tip
Patient troubled by bilateral and seasonal nasal obstruction due to allergies, and morphologically by a wide, drooping tip that worsened when smiling. Examination revealed inferior turbinate hypertrophy, a deviated septum, and internal valve syndrome.
A rhinoseptoplasty combined with radiofrequency treatment of the inferior turbinates was performed six months ago, as usual, without any visible scars.



Nasal Asymmetry Correction and Functional Improvement
This patient was troubled by nasal asymmetry with significant breathing difficulties. In addition to a severe deviation of the septum, there was a dorsal hump and an asymmetrically short tip, resulting in functional issues. A conservative anatomical rhinoplasty was performed a year ago, with no visible scarring and straightforward recovery. Today, she is a happy patient breathing well.



Conservative Anatomical Rhinoplasty and Otoplasty
Our young patient suffered from a rhinoseptal deviation, an osteocartilaginous bump with an overly high and long septum causing significant deviation, and a deviated, undefined tip. She also had asymmetric protruding ears with a folding defect of the auricle, conchal hypertrophy, and lobule protrusion.
The conservative anatomical rhinoplasty (scarless, rhinoseptal realignment, and tip cartilage work) and otoplasty were performed during the same operation under general anesthesia. The postoperative course was simple, with one week of downtime due to the splint. The result, shown here at one year, is very discreet.



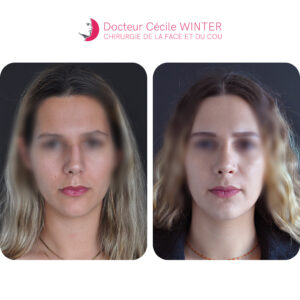
Conservative Anatomical Rhinoplasty
Young patient with a prominent nose featuring a hump, a wide tip, and a pinched middle third, associated with valve syndrome. The root height, the angle between the nose and the mouth, and the infratip are aesthetically pleasing.
The conservative anatomical rhinoplasty aimed to reduce the septal height and the hump, recreate a functional internal valve to improve breathing, and refine the tip to achieve a more feminine nose with a well-defined supratip.
The result is shown at over one year.



Conservative Anatomical Rhinoplasty
Patient presented with a tense nose and a very high septum, causing both internal and external valve syndrome. The tip was suspended and drooping, and the angle between the nose and mouth was quite open. The nasal root height, nasal base height, and actual tip projection were appropriate.
The conservative anatomical rhinoplasty aimed to improve breathing by reducing septal height while maintaining its length and adapting it to the actual tip height. The tip cartilages were also adjusted, as their vertical orientation caused breathing difficulties. They were horizontalized, which better defined the supratip and nostril opening.



Conservative Anatomical Rhinoplasty
Young patient with a rounded tip turned downward, excess septal height (Corbin and internal valve syndrome), and a short nose with insufficient support beneath the tip. The root and base width are good.
A conservative anatomical rhinoplasty was performed to improve the patient's breathing and harmonize her nose with her face. The tip was supported, and the septal height was adjusted to match the actual height of the tip. The cartilages of the tip, initially rounded and vertical, were reshaped and repositioned horizontally to enhance both function and aesthetic appearance.
Result at one and a half years.



Conservative Anatomical Rhinoplasty
Young patient with an asymmetrical nose, internal valve syndrome, a bump, and a moderately defined tip. The infratip, root, and base are aesthetically pleasing. A conservative anatomical rhinoplasty was performed to address the septal deviation, as well as the excess height and length of the septum. The tip was slightly reworked and adjusted to this new height to maintain the infratip and create a well-defined supratip. Once again, the goal of this rhinoplasty is to ensure proper breathing and achieve a nose that is very harmonious with the face, making the surgical work completely unnoticeable. The result is at 2 years.



Conservative Anatomical Rhinoplasty
Young patient with a history of nasal trauma presenting with a bump, rhino-septal deviation, and bilateral nasal obstruction. The entire nose (bridge and tip) was deviated due to the trauma, and the angle between the nose and mouth was very open. Here, the conservative anatomical rhinoplasty performed addressed the nasal obstruction and external signs of trauma by straightening the septum, removing the bump, and readapting and realigning the tip. The challenge was not to shorten the nose while restoring the original harmony of her face. Result is over one year post-op.



Conservative Anatomical Rhinoplasty
Patient presenting with a hyper-projected dorsum with a bump, a pinched dorsum with internal valve syndrome, and a hanging tip. The nasal root is at the right height, the nose is relatively short, and the projection of the tip as well as the infratip are good. The conservative anatomical rhinoplasty performed here involved removing the bump, repositioning the tip, creating a supratip, and making sure not to shorten the nose. The result is seen here at 4 years post-op.









Correction of Nasal Obstruction and Drooping Tip
This young patient was troubled by nasal obstruction, with a broad and downward-rounded tip (Corbin) on the base of a small comma-shaped nose, with a well-placed root and a nice infratip. The conservative anatomical rhinoplasty aimed to improve breathing, lift and refine the tip to create an elegant supra-tip, while minimizing nose reduction to preserve respiratory function. The results are shown at one and a half years post-op.



Correction of Undefined and Drooping Tip
A young patient presented with an undefined, drooping tip and a slightly convex and long dorsum. The central part of the lobule, the root, and the nose-lip distance were aesthetically pleasing. A conservative anatomical rhinoplasty addressed these two morphological issues while maintaining the root height, the attractiveness of the infratip, and redefining the supratip.
The results are shown at one and a half years post-op.